Walgreens just announced its decision to close approximately 1,200 stores across the U.S., adding to growing concerns about the worsening pharmacy desert problem, particularly for the elderly. The closures will take place over the next three years, with 500 stores expected to shutter by the end of fiscal year 2025. For hundreds of thousands of seniors who depend on these locations for prescription medications, vaccines, and other health services, the disappearance of nearby pharmacies poses significant challenges.

This is part of a larger trend in the pharmacy industry, with CVS also planning to shut down 900 stores by the end of 2024, and Rite Aid shutting down over 800 locations as it faces bankruptcy. As more stores close, many communities, particularly those with large elderly populations, are at risk of becoming pharmacy deserts—areas with inadequate access to pharmacies.
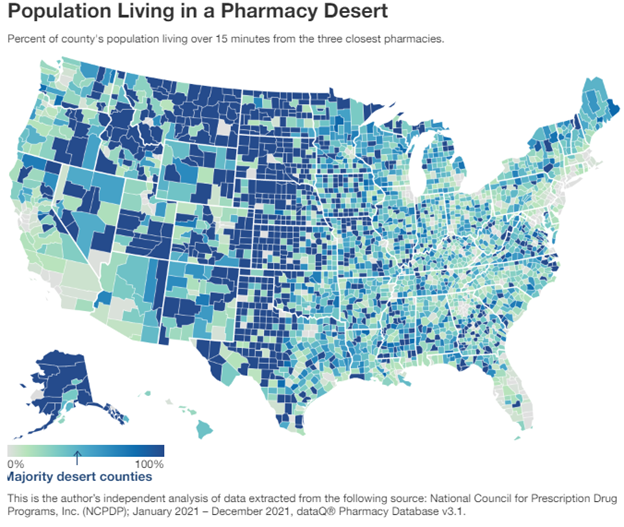
Pharmacy deserts, a term coined in 2014 by Dr. Dima M. Qato, refer to communities where residents struggle to access pharmacy services due to long distances or inadequate transportation options. According to a recent study by GoodRx, over 40% of U.S. counties are considered pharmacy deserts, where people need to travel more than 15 minutes to reach the nearest pharmacy. This lack of access disproportionately affects low-income neighborhoods and older adults who may not drive or have reliable public transportation options.

In cities like Chicago and Los Angeles, pharmacy deserts are increasingly common, and the closure of major chain locations only intensifies the problem. A new interactive mapping tool, developed by the National Community Pharmacists Association (NCPA) and the University of Southern California (USC), highlights the prevalence of pharmacy deserts. It shows that one in three neighborhoods in the 30 largest U.S. cities is a pharmacy desert, with Black and Latino communities hit hardest. Nearly 40% of segregated Black and Latino neighborhoods are classified as pharmacy deserts, compared to 25% of predominantly White neighborhoods.

This lack of access has serious public health implications, particularly for older adults, who are among the most likely to have chronic health conditions and need prescription medications. As nearly 70% of Americans take at least one prescription drug, older patients who live in pharmacy deserts face increasing difficulties in managing their healthcare.

Retailers like Walgreens and CVS have pointed to online ordering and delivery services as a solution for customers in areas impacted by store closures. While this option works well for tech-savvy consumers, it is not a viable solution for many seniors, who are often technologically challenged. A significant portion of the elderly population struggles with online ordering platforms or lacks the necessary devices and internet access to navigate them effectively.

Pharmacy access is critical, not only for medications but also for the rollout of public health initiatives such as vaccines and preventive care. While younger, tech-literate consumers may find online pharmacy services convenient, many seniors don’t have the skills or resources to rely on digital platforms.

Without a user-friendly alternative, many elderly Americans may be left without access to their medications. Traveling long distances to reach a physical pharmacy is not an option for seniors with mobility issues or limited transportation, and public transportation can be unreliable or unavailable in many of these areas.
Another factor driving these closures is the financial pressure faced by pharmacies due to declining reimbursements from Pharmacy Benefit Managers (PBMs). PBMs are responsible for managing prescription drug benefits for insurers and determining reimbursement rates for pharmacies. As reimbursement rates shrink, particularly in rural and low-income urban areas, many pharmacies are forced to close.

The trend of major pharmacy chains closing locations and shifting toward online models may benefit larger corporations, but it comes at the expense of seniors and other vulnerable populations who cannot easily adapt to technological alternatives. As millions of Americans, particularly seniors, face the looming threat of pharmacy deserts, it is clear that relying solely on technological solutions is insufficient. Without immediate action, the growing gap in pharmacy access will continue to impact the health and well-being of the nation’s most vulnerable populations.





