The World Health Organization (WHO) has declared mpox, caused by the monkeypox virus, a “public health emergency of international concern” following a surge in cases across Central Africa. This declaration comes just 15 months after the WHO ended a previous mpox emergency, signaling a renewed threat that the virus could escalate into a global pandemic.
The Africa Centres for Disease Control and Prevention (Africa CDC) also declared a public health emergency on August 13, 2024, as multiple African countries reported their first cases of the disease. The outbreak, which has rapidly spread across the continent, has prompted alarm among scientists and public health officials who fear that the virus could evolve into a more widespread epidemic.
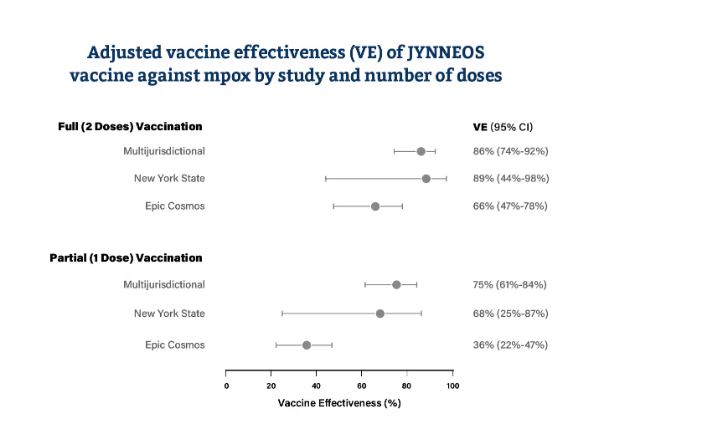
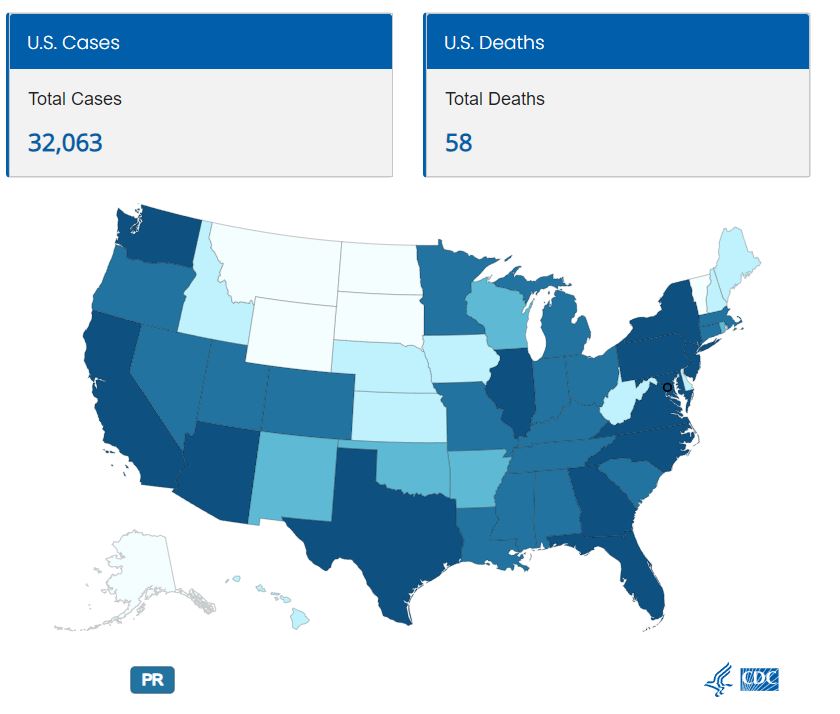
Health officials in several countries, including Canada and the United States, are urging eligible residents to get vaccinated against mpox as cases continue to rise. In British Columbia, the B.C. Centre for Disease Control has recorded 225 confirmed cases since tracking began, with the majority of cases concentrated in the Vancouver Coastal Health area.
In Toronto, a significant spike in mpox cases was recorded in June and July 2024, following summer festivals and events. The city has reported a total of 93 confirmed cases as of July 31, compared to just 21 cases at the same time last year. This rise in cases has raised concerns that mpox could become more prevalent, especially in densely populated areas.

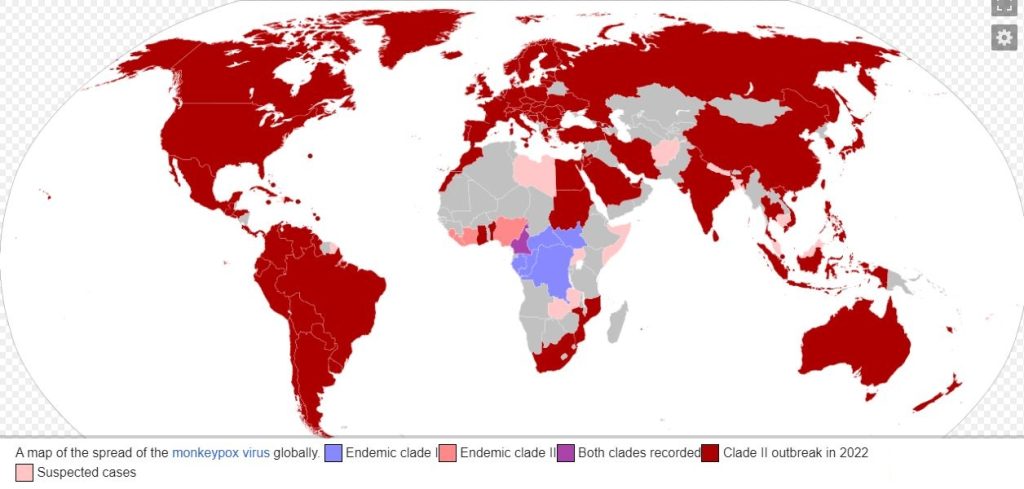
The situation in Africa is particularly concerning. The continent has seen over 17,500 confirmed and suspected mpox infections in 2024 alone, surpassing the total number of cases reported in 2023. The Democratic Republic of the Congo (DRC) has been hit hardest, with nearly 2,400 suspected infections and 56 deaths reported in just one week in early August.
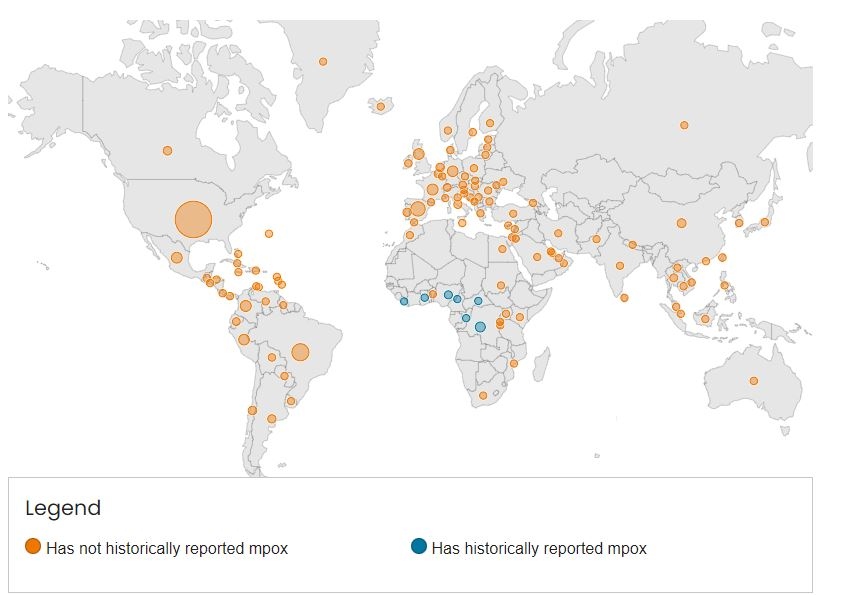
The strain of the monkeypox virus currently circulating in Central Africa is more lethal than the strain responsible for the 2022 global mpox outbreak. This strain, known as clade I, has been spreading rapidly, particularly in regions with poor access to healthcare. The high death rate associated with clade I is attributed to both the virus’s inherent virulence and the challenges of managing outbreaks in rural areas.

The outbreak has spread to neighboring countries, including Burundi, Kenya, Rwanda, and Uganda, all of which have reported their first-ever mpox infections. This spread has been facilitated by highly mobile populations, such as sex workers, who have carried the virus to densely populated areas.
As the virus continues to spread, the Africa CDC is in negotiations to obtain 200,000 doses of the mpox vaccine from Bavarian Nordic, a biotechnology firm based in Denmark. However, this is far short of the 10 million doses that the Africa CDC estimates are needed to control the outbreak. The challenge of delivering these vaccines to regions with poor public health infrastructure and to at-risk populations remains a significant hurdle.
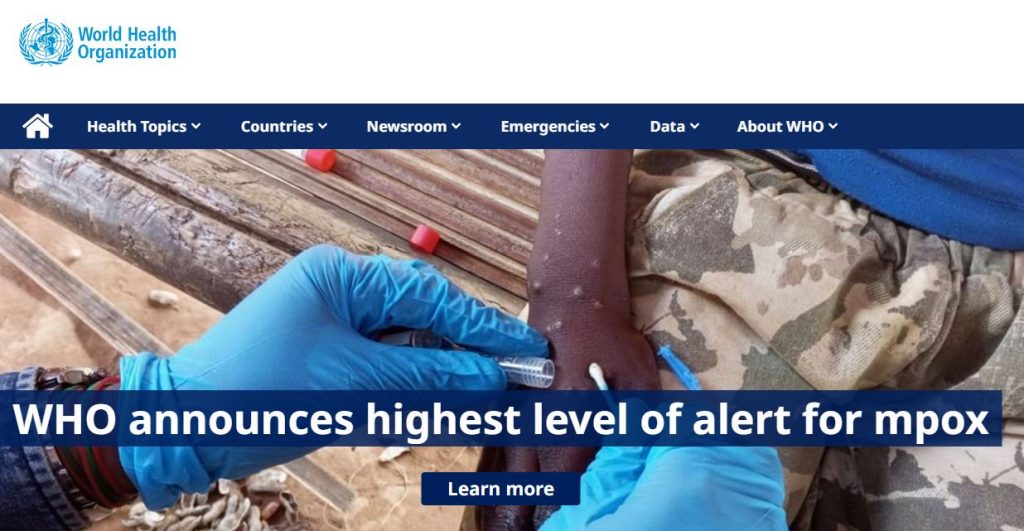
The WHO’s emergency declaration is a call to action for countries around the world to coordinate their efforts to control the mpox outbreak. Rapid surveillance and cooperation between affected countries will be crucial in preventing the virus from becoming the next global pandemic. However, the availability of treatments and vaccines remains a critical issue, particularly in African nations that are currently bearing the brunt of the outbreak.
The potential for Mpox to become a global pandemic underscores the need for a coordinated international response. Public health experts warn that the virus could spread beyond Africa if not contained quickly, making global cooperation and resource allocation essential in the fight against this emerging threat.